Loxitane (Loxapine) Full Prescribing Information
Brand Name: Loxitane
Generic Name: Loxapine
Loxitane (Loxapine) is an antipsychotic medication used to treat schizophrenia. Uses, dosage, side effects of Loxitane.
Outside U.S., Brand Names also known as Loxapac.
Loxitane Full Prescribing Information (PDF)
Description
Pharmacology
Indications and Usage
Contraindications
Warnings
Precautions
Drug Interactions
Adverse Reactions
Overdose
Dosage
Supplied
Description
Loxapine (Loxitane) is an antipsychotic medication used to treat psychosis and disorganized thinking associated with schizophrenia.
Pharmacology
Loxapine is a tricyclic dibenzoxazepine antipsychotic agent, which produces pharmacological responses in various animal species which are characteristic of those seen with the majority of antipsychotic drugs.
The precise mechanism of action is not known. Loxapine succinate administration results in strong inhibition of spontaneous motor activity.
Following oral administration of a single 25 mg dose of loxapine, the onset of sedative effect occurs in 15 to 30 minutes; peak effect occurs within 1-3 hours. The duration of sedative effect is approximately 12 hours.
Indications and Usage
Loxitane is for the symptomatic treatment of schizophrenia.
Contraindications
Loxapine is contraindicated in patients known to be hypersensitive to it.
Comatose or severe drug induced depressed states.
Patients with circulatory collapse.
Warnings
Neuroleptic Malignant Syndrome (NMS): A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) has been reported in association with administration of antipsychotic drugs. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac dysrhythmia). Additional signs may include elevated creatinine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
The management of NMS should include immediate discontinuation of all antipsychotic drugs including olanzapine, intensive monitoring of symptoms and treatment of any associated medical problems.
If a patient requires antipsychotic drug treatment after recovery from NMS, the potential reintroduction of drug therapy should be carefully considered. The patient should be carefully monitored, since recurrences of NMS have been reported.
Tardive Dyskinesia: A syndrome of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
Given these considerations, loxapine should be prescribed in a manner that is most likely to minimize the risk of tardive dyskinesia. As with any antipsychotic drug, olanzapine should be reserved for patients who appear to be receiving substantial benefit from the drug. In such patients the lowest effective dose and the shortest duration of treatment should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient on loxapine, drug discontinuation should be considered. However, some patients may require treatment with loxapine despite the presence of the syndrome.
This drug is not recommended for use in patients suffering from blood dyscrasias or liver disease of significant severity.
Loxapine has not been evaluated for the management of behavioral complications in patients with mental retardation and therefore cannot be recommended in these patients.
Precautions
Seizures: Loxapine should be used with extreme caution in patients with a history of convulsive disorders, since it lowers the convulsive threshold. Seizures have been reported in epileptic patients receiving loxapine at antipsychotic dose levels and may occur even with maintenance of routine anticonvulsant drug therapy.
Cardiovascular: Use loxapine with caution in patients with cardiovascular disease. Increased pulse rate and transient hypotension have both been reported in patients receiving antipsychotic drugs.
Although clinical experience has not demonstrated ocular toxicity, careful observation should be made for pigmentary retinopathy and lenticular pigmentation, since these have been observed in some patients receiving certain other antipsychotic drugs for prolonged periods.
Due to possible anticholinergic action, use loxapine with caution in patients with glaucoma or a tendency to urinary retention, particularly with concomitant administration of antiparkinson medication.
Breast Cancer: Neuroleptic drugs elevate prolactin levels; the elevation persists during chronic administration. Tissue culture experiments indicate that approximately one-third of human breast cancers are prolactin-dependent in vitro, a factor of potential importance if the prescription of these drugs is contemplated in a patient with a previously detected breast cancer. Although disturbances such as galactorrhea, amenorrhea, gynecomastia and impotence have been reported, the clinical significance of elevated serum prolactin levels is unknown for most patients. An increase in mammary neoplasms has been found in rodents after chronic administration of neuroleptic drugs. Neither clinical studies, nor epidemiologic studies conducted to date, however, have shown an association between chronic administration of these drugs and mammary tumorogenesis; the available evidence is considered too limited to be conclusive at this time.
Usage in Children:: Studies have not been performed in children; therefore, this drug is not recommended for use in children below the age of 16.
Pregnancy and Withdrawl: Safe use of loxapine during pregnancy or lactation has not been established; therefore, its use in pregnancy, in nursing mothers or in women of childbearing potential requires that the benefits of treatment be weighed against the possible risks to mother and child.
Interference with Cognitive or Motor Performance: Since loxapine may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks, such as operating an automobile or machinery, the patient should be cautioned accordingly.
Drug Interactions
Loxapine will add to the effects of alcohol and other CNS depressants.
BEFORE USING THIS MEDICINE: INFORM YOUR DOCTOR OR PHARMACIST of all prescription and over-the-counter medicine that you are taking. Inform your doctor of any other medical conditions, including heart or seizure conditions, allergies, pregnancy, or breast-feeding.
Adverse Reactions
The incidence of sedation following loxapine administration has been less than that of certain aliphatic phenothiazines and slightly more than the piperazine phenothiazines. Drowsiness, usually mild, may occur at the beginning of therapy or when dosage is increased. It usually subsides with continued loxapine therapy.
Along with its needed effects, loxapine can sometimes cause serious side effects. Tardive dyskinesia (a movement disorder) may occur and may not go away after you stop using the medicine. Signs of tardive dyskinesia include fine, worm-like movements of the tongue, or other uncontrolled movements of the mouth, tongue, cheeks, jaw, or arms and legs. Other serious but rare side effects may also occur. These include severe muscle stiffness, fever, unusual tiredness or weakness, fast heartbeat, difficult breathing, increased sweating, loss of bladder control, and seizures (neuroleptic malignant syndrome). You and your doctor should discuss the good this medicine will do as well as the risks of taking it.
Stop taking loxapine and get emergency help immediately if any of the following side effects occur: Rare: Convulsions (seizures); difficult or fast breathing; fast heartbeat or irregular pulse; fever (high); high or low blood pressure; increased sweating; loss of bladder control; muscle stiffness (severe); unusually pale skin; unusual tiredness or weakness.
Check with your doctor immediately if any of the following side effects occur: More common: Lip smacking or puckering; puffing of cheeks; rapid or fine, worm-like movements of tongue; uncontrolled chewing movements; uncontrolled movements of arms or legs.
Also, check with your doctor as soon as possible if any of the following side effects occur: More common (occurring with increase of dosage): Difficulty in speaking or swallowing; loss of balance control; mask-like face; restlessness or desire to keep moving; shuffling walk; slowed movements; stiffness of arms and legs; trembling and shaking of fingers and hands.
Less common: Constipation (severe); difficult urination; inability to move eyes; muscle spasms, especially of the neck and back; skin rash; twisting movements of the body.
Rare: Sore throat and fever; increased blinking or spasms of eyelid; uncontrolled twisting movements of neck, trunk, arms, or legs; unusual bleeding or bruising; unusual facial expressions or body positions; yellow eyes or skin
Other sides effects include: Blurred vision; confusion; dizziness, lightheadedness, or fainting; drowsiness; dryness of mouth, constipation (mild); decreased sexual ability; enlargement of breasts (males and females); headache; increased sensitivity of skin to sun; missing menstrual periods; nausea or vomiting; trouble in sleeping; unusual secretion of milk; weight gain.
Drug Abuse and Dependence
Abrupt withdrawal after short-term administration of antipsychotic drugs does not generally pose problems. However, transient dyskinetic signs are experienced by some patients on maintenance therapy after abrupt withdrawal. The signs are very similar to those described under Tardive Dyskinesia, except for duration. Although it is not known whether gradual withdrawal of antipsychotic drugs will decrease the incidence of withdrawal emergent neurological signs, gradual withdrawal would appear to be advisable.
Overdose
Signs and Symptoms
Symptoms of an overdose are dizziness (severe); drowsiness (severe); unconsciousness; muscle trembling, jerking, stiffness, or uncontrolled movements (severe); troubled breathing (severe); unusual tiredness or weakness (severe).
Other symptoms of overdose may include flushing, dry mouth, drowsiness, confusion, agitation, enlarged pupils, seizures.
Renal failure following loxapine overdosage has also been reported.
Treatment
If you or someone you know may have used more than the recommended dose of this medicine, contact your local poison control center or emergency room immediately.
No specific antidote is known.
Maintain adequate airway, empty stomach contents, and treat symptomatically.
Dosage
Do not exceed the recommended dosage or take this medicine for longer than prescribed.
- Follow the directions for using this medicine provided by your doctor.
- Store this medicine at room temperature, in a tightly-closed container, away from heat and light.
- If you miss a dose of this medicine, take it as soon as possible. If it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not take 2 doses at once.
Additional Information:: Do not share this medicine with others for whom it was not prescribed. Do not use this medicine for other health conditions. Keep this medicine out of the reach of children.
This medicine may be taken with food or a full glass (8 ounces) of water or milk to reduce stomach irritation. The liquid medicine must be mixed with orange juice or grapefruit juice just before you take it to make it easier to take.
The dose of loxapine will be different for different patients.
This medication is not recommended for children under the age of 16 years.
For oral dosage forms (capsules, oral solution, or tablets):
Adults: To start, 10 milligrams taken two times a day. Your doctor may increase your dose if needed. The usual therapeutic range is 60 to 100 mg daily. However, as with other antipsychotic drugs, some patients respond to lower dosage and others require higher dosage for optimal benefit. Daily dosage higher than 250 mg is not recommended.
Maintenance Dosage: Reduce dosage to the lowest level compatible with symptom control. Many patients maintain satisfactorily at dosages in the range of 20 to 60 mg daily.
For injection dosage form:
Adults: 12.5 to 50 milligrams every four to six hours, injected into a muscle.
How Supplied
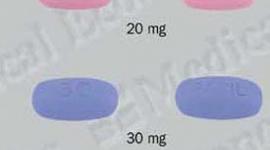
Tablets: (and available in capsule form in these dosages): 5 mg, 10 mg, 50 mg.
Injectable: Each 1 mL ampul contains: Loxapine HCl equivalent to loxapine 50 mg for i.m. injection. Tartrazine-free. Boxes of 10.
Oral Concentrate: Each mL of clear, colorless solution (pH: 5.0 to 7.0) contains: Loxapine 25 mg as loxapine HCl. Should be mixed with orange or grapefruit juice shortly before administration. Use only the enclosed calibrated (10, 15, 25 or 50 mg) dropper and calibrated 2.5, 5.0, 7.5, 10.0, 12.5 or 15.0 mg) syringe for dosage. Bottles of 100 mL.
IF USING THIS MEDICINE FOR AN EXTENDED PERIOD OF TIME, obtain refills before your supply runs out.
Loxitane Full Prescribing Information (PDF)
Detailed Info on Signs, Symptoms, Causes, Treatments of Schizophrenia
The information in this monograph is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects. This information is generalized and is not intended as specific medical advice. If you have questions about the medicines you are taking or would like more information, check with your doctor, pharmacist, or nurse. Last updated 3/03.
Copyright © 2007 Healthyplace Inc. All rights reserved.
APA Reference
Staff, H.
(2009, January 3). Loxitane (Loxapine) Full Prescribing Information, HealthyPlace. Retrieved
on 2024, June 20 from https://www.healthyplace.com/other-info/psychiatric-medications/loxapine-loxitane-full-prescribing-information